Overview
This article addresses a crucial aspect of diabetes management: the essential billing codes for Continuous Glucose Monitoring (CGM). It’s important to recognize that understanding and utilizing CPT codes 95250, 95251, and 95249 can significantly impact healthcare providers’ ability to secure proper reimbursement. By doing so, they enhance patient care, which is vital for those navigating the challenges of diabetes.
Many patients find that these codes facilitate the billing process for both professional and personal use of CGMs. This understanding not only streamlines the administrative side of care but also contributes to improved health outcomes for individuals managing diabetes. As we explore these billing codes, let’s remember that they play a pivotal role in ensuring that patients receive the support they need on their journey to better health.
Introduction
In the realm of diabetes management, it’s important to recognize how technology has transformed the way patients monitor and understand their health. The introduction of Continuous Glucose Monitoring (CGM) systems offers real-time insights into glucose levels, empowering individuals to make informed dietary and lifestyle choices.
However, many patients find that navigating the complexities of CGM utilization, including billing practices and insurance coverage, can be challenging.
This article delves into the multifaceted landscape of CGM, exploring essential CPT codes, reimbursement strategies, and the transformative impact of remote patient monitoring.
By shedding light on these critical components, we aim to enhance understanding and accessibility of CGM technology, ultimately fostering better health outcomes for those living with diabetes. Together, we can navigate this journey toward improved health.
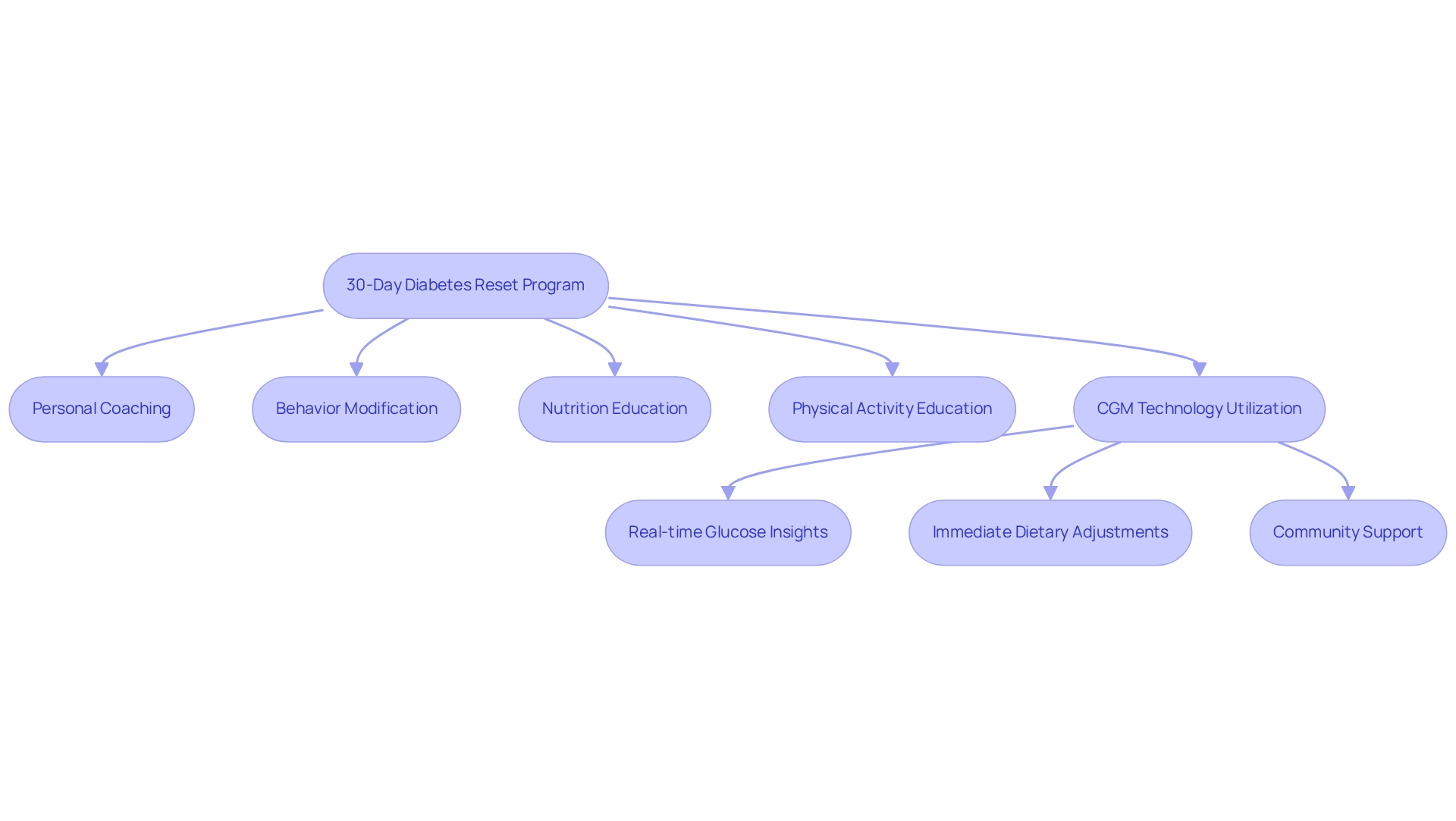
Integrative Wellness Center: 30-Day Diabetes Reset Program for Effective CGM Utilization
The Integrative Wellness Center’s 30-Day Diabetes Reset Program is thoughtfully designed to empower individuals with the essential tools and knowledge needed to effectively utilize continuous glucose monitoring (CGM) technology, as well as understand CGM billing codes. It’s important to recognize that managing diabetes can be challenging, and this program emphasizes personalized coaching, behavior modification, and comprehensive education on nutrition and physical activity. By seamlessly integrating CGM technology, patients gain real-time insights into their glucose levels, enabling immediate dietary and lifestyle adjustments.
Many patients find that CGMs provide real-time updates on blood glucose levels, significantly enhancing their ability to manage the condition. This proactive strategy minimizes the need for frequent finger pricks and allows for immediate corrective actions. Not only does this improve management of the condition, but it also fosters a deeper understanding of how daily choices affect blood sugar levels. One individual shared, “I was depressed, no energy, and had insomnia. I was on two different meds that weren’t working… After starting this program, I lost 55 lbs, and my A1C improved from 9.1 to 5.7 in just 8 months.”
Participants often experience significant improvements in their health outcomes, underscoring the program’s effectiveness in fostering long-term wellness. Furthermore, health disparities related to CGM billing codes and access to continuous glucose monitoring, particularly in minority communities, highlight the importance of this program in addressing the needs of underserved populations. As K.E., a health professional, mentioned, “The incorporation of CGM billing codes is essential for managing blood sugar levels and enabling individuals to take charge of their health.” This program is not just about technology; it’s about creating a supportive community that understands and addresses your unique journey.
CPT Code 95250: Professional Use of Continuous Glucose Monitors
CPT Code 95250 plays a vital role in the professional application of Continuous Glucose Monitors (CGMs), encompassing the essential setup, calibration, and initial user instruction needed for effective blood sugar management. This code is applicable when healthcare professionals conduct ambulatory continuous glucose monitoring of interstitial tissue fluid through a subcutaneous sensor for a minimum of 72 hours. By utilizing this code, providers can secure reimbursement for the time and resources dedicated to individual education and monitoring—key components in managing this condition effectively.
It’s important to recognize that integrating holistic health solutions, like those advocated by Dr. Jason Shumard, underscores the significance of lifestyle modifications alongside CGM technology. For example, engaging in regular outdoor activities in San Marcos, CA, can greatly enhance insulin sensitivity and overall health. Many patients find that ongoing support is crucial; recent statistics reveal that 63.2% continued to utilize professional Continuous Glucose Monitoring (p-CGM) during a six-month follow-up, highlighting the importance of consistent monitoring in managing blood sugar levels. A compelling case study illustrates this impact: a 75-year-old African-American man with newly diagnosed type 2 hyperglycemia, initially presenting an A1C of 10.5%, achieved an A1C of 5.9% and ceased all prescribed medications after participating in a program that combined CGM use with lifestyle changes.
Moreover, individuals receive a copy of their CGM report for personal records and ongoing management, emphasizing the importance of individual involvement and self-management in glucose care. The professional setup of CGMs not only enhances patient education but also significantly improves health outcomes related to blood sugar management. As healthcare providers are increasingly encouraged to embrace p-CGM technology to enhance care for those facing blood sugar challenges in primary settings, understanding the nuances and reimbursement processes associated with CGM billing codes becomes essential for optimizing care. The upcoming updates for this code in 2025 further underscore the relevance of CGM billing codes in contemporary management strategies for blood sugar conditions, reinforcing the need for personalized functional medicine approaches that incorporate tailored nutrition and community support. We extend our gratitude to Dr. David Price for his invaluable feedback on the data analysis and critical review of this manuscript, highlighting the collaborative effort in advancing diabetes care.
CPT Code 95251: CGM Analysis and Interpretation Billing
CPT Code 95251 plays a crucial role in CGM billing codes for the analysis and interpretation of data gathered from Continuous Glucose Monitors (CGMs). This code becomes relevant when a healthcare professional reviews at least 72 hours of CGM data and produces a comprehensive report tailored to the individual. Accurate billing under CGM billing codes is essential, as it enables healthcare providers to receive compensation for the vital analysis that informs treatment adjustments, ultimately improving outcomes for individuals. It’s worth noting that routine DMS utilized by home health providers is included in the reimbursement rate for these services, highlighting the broader implications of CPT Code 95251 in the reimbursement framework for blood sugar management.
Recognizing patterns in glucose levels through CGM data empowers healthcare providers to make timely adjustments to an individual’s management plan. Many patients find that effective use of CGM data leads to better glycemic control and overall health improvements. For instance, a case study of a 75-year-old man with newly diagnosed type 2 diabetes illustrates this point. After engaging in a structured management program, he successfully reversed his dysglycemia, achieving an impressive A1C reduction from 10.5% to 6.2% without medication. This example underscores the importance of the analysis and interpretation process associated with CPT Code 95251, directly linking it to positive patient outcomes.
In addition to CGM data analysis, Dr. Jason Shumard’s book on reversing type 2 diabetes offers invaluable insights and strategies for individuals seeking to manage their condition holistically. Participating in our upcoming events can further enhance individual involvement and education, providing additional resources to assist in managing blood sugar levels. Expert opinions emphasize the significance of CPT Code 95251 in blood sugar management, showcasing its role in fostering individual engagement and enabling personalized care. As one vendor noted, “Clinical data models have not historically considered the individual as a direct contributor to the medical record, which has necessitated significant thought and IP investment around how best to store and maintain provenance across concepts.” This evolving perspective highlights the importance of individual information in managing blood sugar conditions.
The growing use of CGM billing codes among healthcare practitioners, particularly CPT Code 95251, reflects its increasing recognition as a vital component of effective blood sugar management. As healthcare continues to evolve, understanding the analysis and interpretation process tied to CGM billing codes will be essential for practitioners aiming to enhance care through data-driven insights. Patients are encouraged to discuss the application of CPT Code 95251 with their healthcare providers to ensure they receive comprehensive diabetes management. Furthermore, exploring resources such as Dr. Shumard’s book and engaging in events can empower individuals on their journey toward better health.
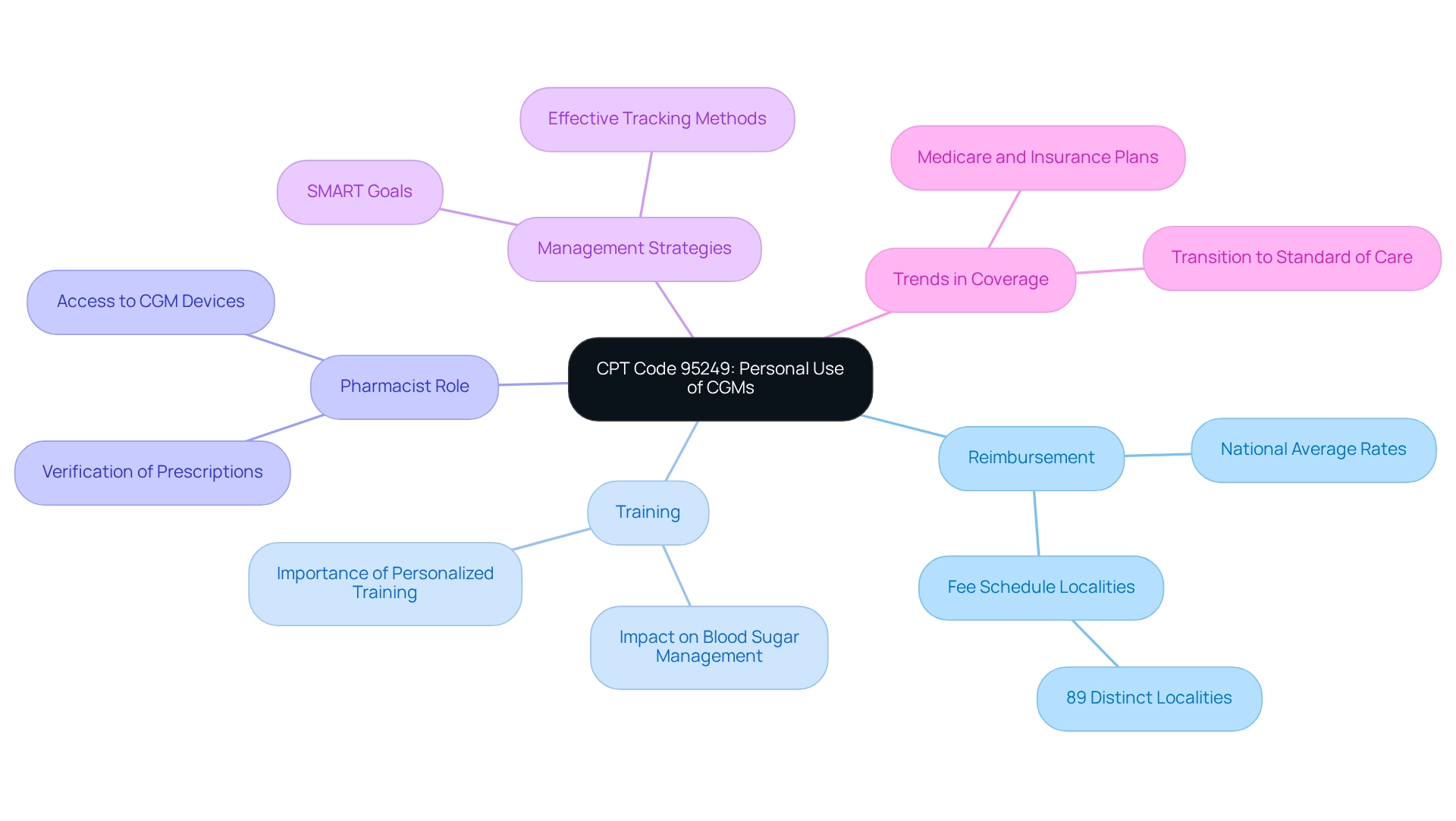
CPT Code 95249: Personal Use of Continuous Glucose Monitors
CPT Code 95249 is designed specifically for the personal use of Continuous Glucose Monitors (CGMs). This code applies when individuals use their own devices for ongoing glucose level monitoring. It encompasses the initial setup, training, and calibration of the CGM, which are vital for effectively managing diabetes at home. Understanding CPT Code 95249 is essential for those seeking reimbursement for their personal CGM devices, as it enables easier access to these crucial tools.
It’s important to recognize that navigating the reimbursement landscape can be complex. Recent statistics reveal that there are 89 distinct fee schedule localities across the country for CGM billing codes. National average reimbursement rates for CGM billing codes provide valuable insights into the financial aspects of using these devices. As the approach to blood sugar management evolves, Medicare and other insurance plans are increasingly acknowledging the significance of CGMs, expanding coverage for both personal and professional use. Many patients find that standardized CGM reports enhance their understanding of the factors affecting their glucose levels, supporting the transition of CGMs toward becoming the new standard of care in diabetes management.
Furthermore, pharmacists now have the authority to verify prescriptions for conventional blood glucose monitoring supplies when prescribing CGM devices. This change simplifies the process for individuals, making it easier to access the support they need. As reimbursement trends for personal CGM usage continue to evolve, it is crucial for individuals to stay informed about CGM billing codes and the significance of CPT Code 95249. Diabetes instructors emphasize the importance of personalized training for CGM devices, highlighting that adequate education can greatly influence blood sugar management at home.
By implementing effective tracking methods and setting SMART goals—specific, measurable, attainable, relevant, and time-bound—patients can enhance their focus and motivation in managing their condition. Dr. Jason Shumard states, “By providing individuals with actionable insights and practical tools, the center fosters an environment where they can reclaim their health and well-being, ultimately leading to improved quality of life and reduced reliance on conventional medical interventions.” This comprehensive approach is vital for the efficient management of blood sugar levels.
Billing Guidelines for Wearable Continuous Glucose Monitors
Billing for wearable Continuous Glucose Monitors (CGMs) can feel overwhelming, but understanding the CGM billing codes is key to securing proper reimbursement. It’s essential to document medical necessity clearly, outlining the reasons for prescribing the device. By thoroughly documenting individual education, providers demonstrate their commitment to empowering individuals on their health management journey. This empowerment is further enhanced by personalized guidance from experts like Dr. Jason Shumard, who emphasizes holistic lifestyle strategies tailored to individual needs.
It’s important to recognize that accurate coding of all services rendered is crucial to avoid claim denials. Statistics suggest that comprehensive documentation can greatly decrease claim denials, with efficient practices leading to better outcomes for individuals. For instance, home temperature evaluation of the foot has been shown to reduce the occurrence of foot ulcers by ten times compared to standard preventive care. This underscores the significance of efficient monitoring and record-keeping in managing diabetes-related conditions.
Many patients find that a comprehensive approach to health—one that focuses on individualized care and education—can vastly improve their quality of life while reducing dependence on traditional medical treatments. Expert advice highlights that common challenges in CGM reimbursement often stem from insufficient documentation or misunderstandings of CGM billing codes. As noted by Rayman et al., sensor-based glucose information with directional arrows offers distinct advantages over traditional blood glucose testing, supporting safe glucose levels associated with driving. To navigate these complexities, practitioners are encouraged to adopt best practices for CGM billing codes documentation, ensuring that all necessary information is included to support claims. By following these guidelines, healthcare professionals can help improve access to CGM technology for their patients, ultimately enhancing diabetes management and patient satisfaction.
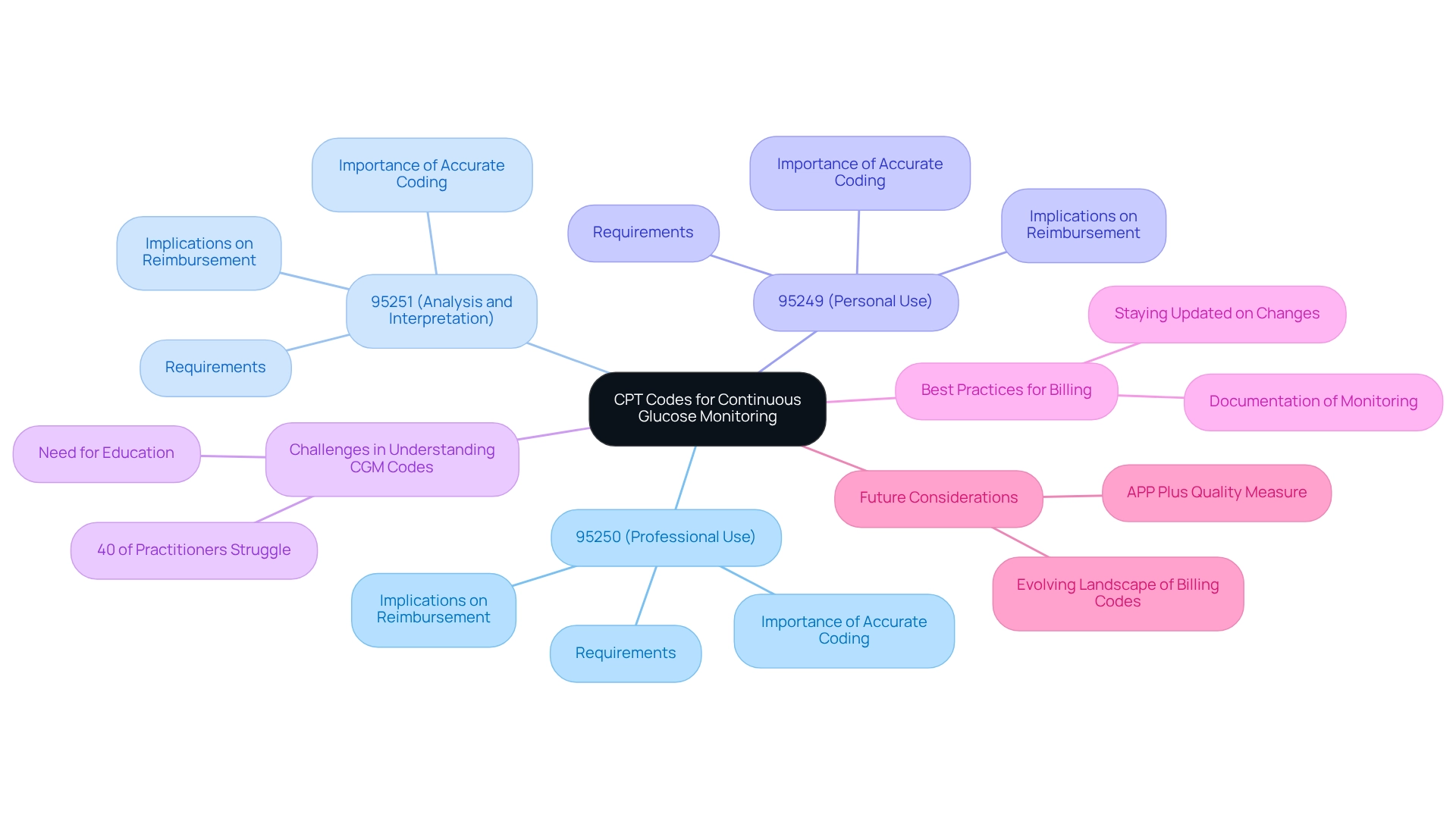
Deciphering CPT Codes for Continuous Glucose Monitoring
Understanding the cgm billing codes for Continuous Glucose Monitoring (CGM) is crucial for healthcare professionals who are striving for accurate billing and optimal reimbursement. The primary codes include:
- 95250, which pertains to professional use
- 95251 for analysis and interpretation
- 95249 for personal use
Each code has specific requirements, such as the minimum duration of monitoring and the type of service provided, which are essential for compliance and reimbursement.
It’s important to recognize that precise coding directly influences reimbursement rates. Practitioners must grasp these distinctions to ensure they receive appropriate compensation for their services. A recent survey revealed that around 40% of practitioners struggle to understand CGM CPT codes, underscoring the urgent need for education in this area to avoid billing errors and delayed payments.
Statements from healthcare billing specialists further emphasize the importance of accurate coding: ‘Grasping the intricacies of CPT codes is vital for professionals to guarantee they are reimbursed appropriately for their services,’ notes a prominent billing consultant. Many healthcare providers have shared real-world examples that illustrate effective billing practices for CGM services. Those who carefully document the duration and context of monitoring often report fewer claim denials and improved cash flow; additionally, staying updated on the recent changes in cgm billing codes is essential, as the landscape is continually evolving to reflect advancements in technology and care practices.
Navigating the billing process for CGM services can be intricate, but understanding cgm billing codes empowers practitioners to advocate effectively for their services. Engaging with case studies, such as the recent feedback on APCM Services Valuation, can illuminate best practices, ensuring healthcare professionals are compensated fairly for the comprehensive care they provide. Furthermore, with the proposed APP Plus quality measure set to begin in the CY 2025 performance period, it is crucial for providers to remain informed about the evolving landscape of cgm billing codes and their implications.
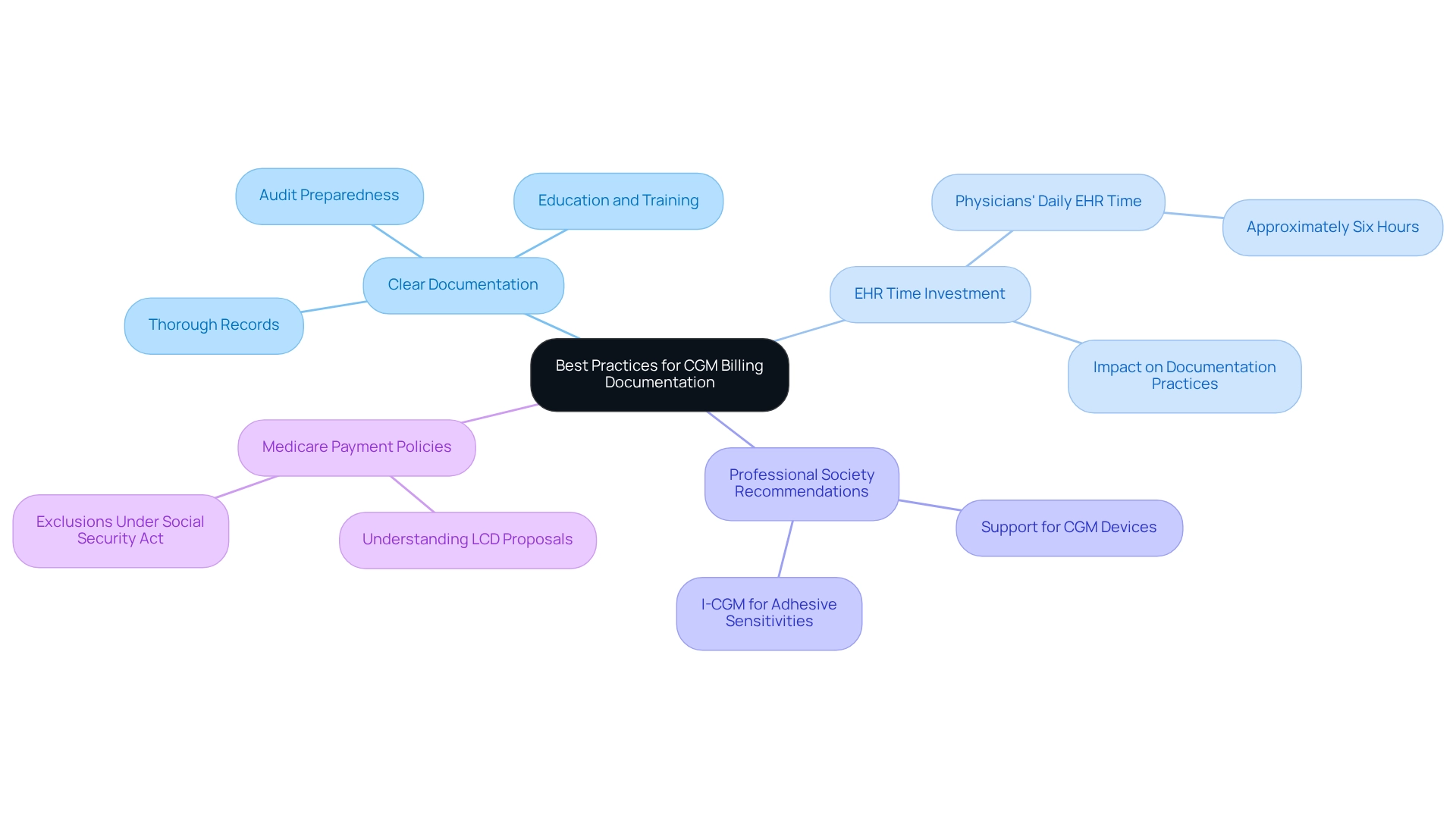
Best Practices for CGM Billing Documentation
Effective documentation for CGM billing codes is built upon thorough records that encompass interactions, device usage, and any adjustments to treatment plans guided by CGM data. It’s important to recognize that providers must ensure all documentation is clear, concise, and easily accessible for potential audits. Detailed notes on individual education and training concerning CGM use are essential, as they not only strengthen assertions but also validate the medical necessity of the services provided. By following these best practices, healthcare professionals can significantly enhance their chances of successful reimbursement.
Statistics indicate that physicians dedicate approximately six hours daily to electronic health record (EHR) data entry, which includes clinical documentation and billing functions. This highlights the necessity for meticulous documentation practices in CGM billing codes, as thorough records can directly influence the outcomes of reimbursement. Many patients find that various professional societies advocate for the use of continuous glucose monitoring (CGM) devices, reinforcing the importance of proper documentation in supporting their medical necessity. For instance, recommendations from professional societies highlight the potential of I-CGM as an alternative for individuals with sensitivities to traditional CGM adhesives, emphasizing the need for adherence to established guidelines.
Furthermore, understanding Medicare payment policies for I-CGM devices is crucial for practitioners to efficiently manage the complexities of CGM billing codes. The proposed LCD emphasizes the importance of staying informed about these policies, which is essential for successful documentation. As Dr. Jason Shumard states, “By providing individuals with actionable insights and practical tools, the center fosters an environment where they can reclaim their health and well-being, ultimately leading to improved quality of life and reduced reliance on conventional medical interventions.” By implementing these strategies, providers can navigate the complexities of CGM billing codes more effectively, ultimately benefiting both their practice and those they serve.
Understanding Reimbursement for Continuous Glucose Monitoring Services
Navigating reimbursement for Continuous Glucose Monitoring (CGM) services can be challenging, especially when understanding the various CGM billing codes and payer policies regarding medical necessity. Providers must familiarize themselves with Medicare and Medicaid guidelines, along with private insurance policies and CGM billing codes, to ensure compliance and optimize reimbursement opportunities. Key aspects include:
- Understanding the frequency of CGM billing codes
- The types of services covered
- The documentation requirements necessary for successful claims related to CGM billing codes
Many patients find that maintaining an A1C of less than 7% (53 mmol/mol) is crucial for their health. This highlights the importance of effective management tools for blood sugar levels, such as CGM. Additionally, managed care professionals are increasingly recognizing the transformative potential of CGM in diabetes management. They advocate for informed coverage decisions that align with value-based care goals. As noted by M.E.L., identifying populations with lower-than-expected utilization is a necessary first step in developing targeted interventions to increase CGM uptake and ultimately improve diabetes-related outcomes.
It’s essential to stay informed about updates in reimbursement policies to maintain a sustainable practice. Real-world examples illustrate the challenges and successes in navigating payer policies for CGM billing codes related to reimbursement. This emphasizes the need for providers to adapt to evolving guidelines. Implementing best practices around CGM coverage, as highlighted in the case study titled ‘Best Practices for Managed Care Pharmacy,’ can significantly enhance health outcomes. Expert opinions from insurance specialists further highlight strategies to maximize reimbursement for CGM billing codes, ensuring that patients receive the necessary support for their diabetes management. Additionally, comprehending the existing reimbursement rates for CGM billing codes among various payers is vital for practitioners to efficiently maneuver through the reimbursement environment.
Insurance Coverage Considerations for CGM Billing
Navigating insurance coverage for Continuous Glucose Monitoring (CGM) devices can be a daunting task, and it’s essential for healthcare providers to understand the specific criteria required for coverage. Many individuals face challenges with their blood sugar management, and documentation of medical necessity is a key element, often requiring a thorough record of their management history. Providers should proactively communicate with individuals about their insurance benefits, including any potential out-of-pocket expenses related to CGM devices and services, ensuring they feel supported in their journey.
It’s important to recognize that recent studies show the use of CGM can significantly reduce A1c levels and glycemic variability in individuals with type 2 diabetes. This underscores the importance of access to these devices. However, many patients find the complexities of insurance coverage challenging. For instance, among adults aged 18-64 with blood sugar issues, many indicated they possess solely private insurance, while older individuals often have Medicare alongside private coverage. This highlights the varied landscape of healthcare coverage that can impact access to CGM, and to effectively advocate for individuals, practitioners should familiarize themselves with the CGM billing codes related to CGM devices. Typically, this involves stipulations such as a documented history of managing blood sugar levels and proof of the necessity for continuous monitoring. Many patients find that understanding the subtleties of CGM billing codes empowers them to convey these advantages clearly to clients, ensuring they are aware of their choices and feel confident in their healthcare decisions. Advocates for individuals emphasize the significance of comprehending insurance benefits, as this awareness can greatly influence a person’s ability to obtain essential resources for managing their condition. To improve communication, professionals might consider developing a straightforward guide or checklist that details essential insurance benefits associated with CGM. This can be distributed during consultations, offering individuals a tangible resource. By equipping themselves with this information, professionals can better assist those they serve in navigating the insurance landscape, ultimately facilitating access to CGM services that are vital for effective diabetes care.
Impact of Remote Patient Monitoring on CGM Billing Practices
The rise of remote individual monitoring has profoundly influenced billing practices for Continuous Glucose Monitoring (CGM) services. As the healthcare landscape increasingly embraces telehealth solutions, it’s important to recognize that practitioners are compelled to revise their billing strategies. This means incorporating traditional CGM billing codes alongside remote monitoring codes. Such adaptations require a thorough understanding of how to document remote interactions effectively and ensure that all services rendered are accurately coded. By embracing these changes, healthcare providers can significantly enhance individual engagement and improve management outcomes for those with blood sugar issues.
Statistics show that the market for remote health monitoring was valued at USD 1.45 billion in 2021 and is expected to reach USD 4.07 billion by 2030, indicating a strong growth rate of 8.74% CAGR. This trend highlights the significance of incorporating remote monitoring into care for individuals managing blood sugar issues. Not only does it simplify billing practices, but it also encourages a more proactive approach to health, which can be incredibly empowering.
Many patients find that successful integration of remote monitoring codes in diabetes management has been demonstrated through various case studies. For instance, a San Diego-based clinic reported a 30% increase in adherence to monitoring protocols after implementing remote billing codes. Experts in telehealth emphasize the necessity of adapting billing strategies, including CGM billing codes, to accommodate these innovations. This ensures that healthcare providers can leverage the full potential of remote monitoring technologies. Dr. Jason Shumard observes, “By offering individuals with actionable insights and practical tools, the center encourages a setting where people can reclaim their health and well-being, ultimately resulting in enhanced quality of life and decreased dependence on traditional medical interventions.” This comprehensive method corresponds with the center’s goal to enable individuals in handling their condition efficiently. By doing so, providers can offer comprehensive care that aligns with the evolving needs of patients managing diabetes.
Conclusion
Integrating Continuous Glucose Monitoring (CGM) technology into diabetes management has truly been a transformative experience for many patients. It offers real-time insights that empower individuals to make informed decisions about their health. By exploring essential CPT codes like 95249, 95250, and 95251, we can see how important proper billing practices and reimbursement strategies are in making CGM devices more accessible. With the right documentation and a clear understanding of medical necessity, healthcare providers can enhance patient outcomes and support individuals in managing their diabetes more effectively.
It’s important to recognize that the Integrative Wellness Center’s 30-Day Diabetes Reset Program exemplifies how personalized coaching and education can lead to significant health improvements. The success stories of participants highlight the necessity of combining technology with holistic approaches to achieve sustainable health outcomes. Many patients find that addressing health disparities and ensuring access to CGM technology for underserved communities is crucial for equitable healthcare solutions.
As we navigate the evolving landscape of diabetes care, understanding the complexities of CGM utilization and reimbursement becomes vital for both providers and patients. Staying informed about insurance coverage considerations and emerging trends in remote patient monitoring allows healthcare professionals to adapt their practices to better serve their patients’ needs. Ultimately, our commitment to empowering individuals through education, technology, and personalized care fosters a more effective and compassionate approach to diabetes management. Together, we can pave the way for improved health and quality of life for those living with this condition.
Frequently Asked Questions
What is the 30-Day Diabetes Reset Program?
The 30-Day Diabetes Reset Program is designed to empower individuals with tools and knowledge to effectively use continuous glucose monitoring (CGM) technology, understand CGM billing codes, and receive personalized coaching, behavior modification, and education on nutrition and physical activity.
How does continuous glucose monitoring (CGM) benefit diabetes management?
CGM provides real-time updates on blood glucose levels, allowing for immediate dietary and lifestyle adjustments. This reduces the need for frequent finger pricks and enhances understanding of how daily choices affect blood sugar levels.
What kind of outcomes can participants expect from the program?
Participants often experience significant health improvements, including weight loss and lower A1C levels. For example, one individual lost 55 lbs and improved their A1C from 9.1 to 5.7 in eight months after starting the program.
How does the program address health disparities related to CGM access?
The program highlights the importance of CGM billing codes and access to continuous glucose monitoring, particularly for underserved populations, ensuring that everyone can manage their diabetes effectively.
What role do CPT Codes 95250 and 95251 play in CGM billing?
CPT Code 95250 is for the setup, calibration, and initial user instruction of CGMs, while CPT Code 95251 is for the analysis and interpretation of CGM data. Both codes are essential for securing reimbursements and improving diabetes management outcomes.
How can lifestyle modifications enhance the effectiveness of CGM technology?
Engaging in regular activities, such as outdoor exercises, can improve insulin sensitivity and overall health, complementing the use of CGM technology for better blood sugar management.
What is the importance of ongoing support in diabetes management?
Ongoing support is crucial for effective management, as evidenced by statistics showing that 63.2% of participants continued to use professional Continuous Glucose Monitoring (p-CGM) during a six-month follow-up.
How does the program support individual involvement in glucose care?
Participants receive a copy of their CGM report for personal records, emphasizing the importance of self-management and individual involvement in their diabetes care journey.
Why is understanding CGM billing codes important for healthcare providers?
Understanding CGM billing codes allows healthcare providers to receive compensation for the time and resources dedicated to patient education and monitoring, which are vital for effective diabetes management.
How can individuals further their education on managing diabetes?
Individuals can explore resources such as Dr. Jason Shumard’s book on reversing type 2 diabetes and participate in upcoming events to enhance their knowledge and skills in managing blood sugar levels.