Overview
Living with Type 2 diabetes can be overwhelming, and it’s crucial to be aware of the signs that your body may be sending you. Here are ten symptoms that should never be overlooked:
- Frequent urination
- Excessive thirst
- Blurred vision
- Fatigue
- Slow healing wounds
- Unexplained weight loss
- Increased hunger
- Dark patches of skin
Recognizing these symptoms is vital, as they are closely linked to diabetes and can significantly impact your health.
It’s important to recognize that early detection and management can make a world of difference. Each symptom serves as a reminder of the need for regular check-ups and proactive health measures. Many patients find that understanding these signs not only empowers them but also leads to timely medical intervention, ultimately improving their health outcomes.
If you or someone you know is experiencing these symptoms, take a moment to reflect on your health. Seeking guidance from a healthcare professional can provide clarity and support. Remember, you are not alone on this journey, and there are resources available to help you regain control over your health.
Introduction
Recognizing the symptoms of type 2 diabetes is crucial for effective management and prevention of complications. It’s important to understand that nearly half of adults with elevated blood sugar levels remain undiagnosed. By recognizing these signs, you can empower yourself to take proactive steps toward your health. This article delves into ten key symptoms of type 2 diabetes that should not be overlooked. What if ignoring these warning signs could lead to more severe health issues down the road? Let’s explore their implications and the importance of early intervention together.
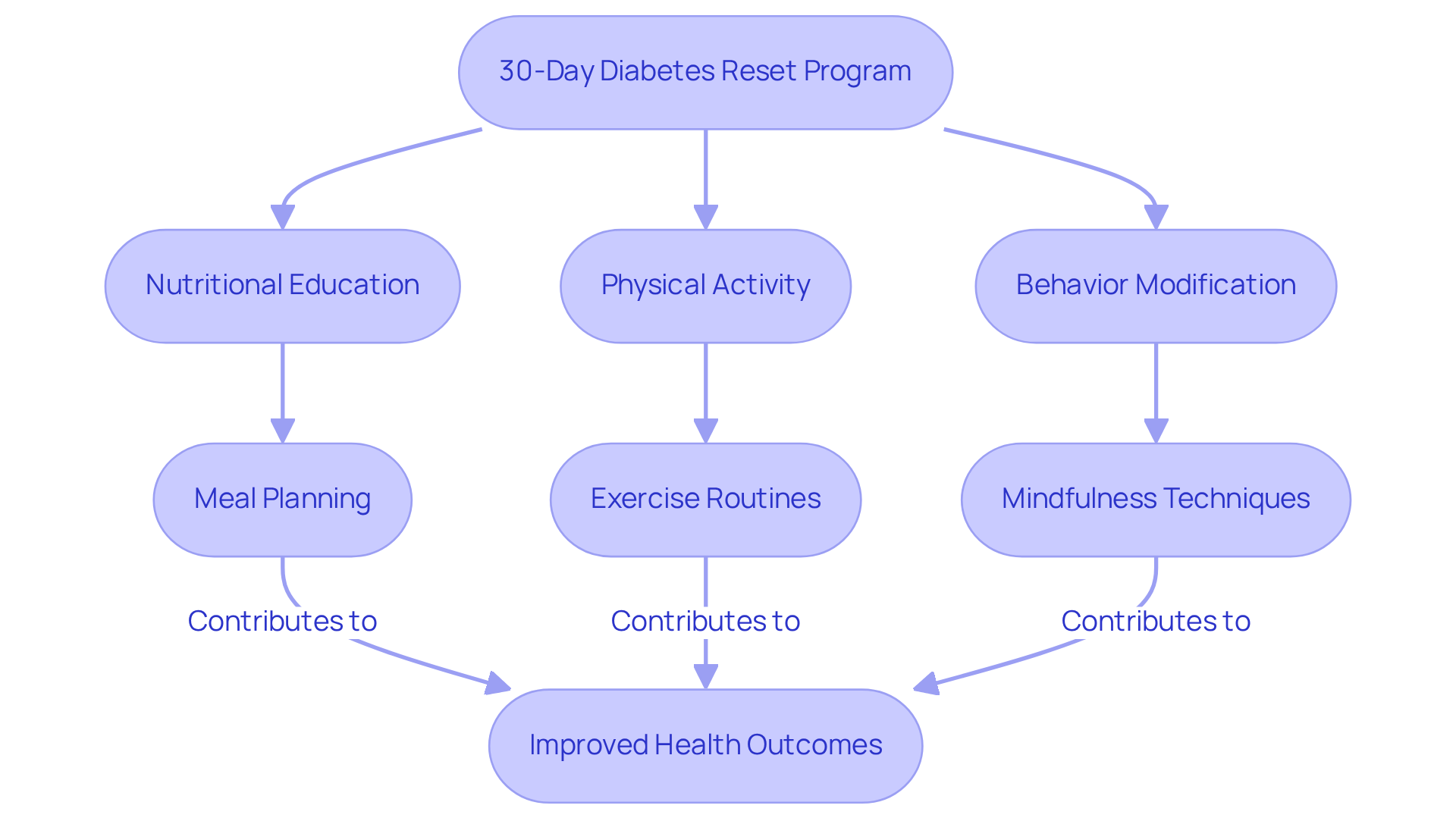
Integrative Wellness Center: 30-Day Diabetes Reset Program for Lasting Health Transformation
Are you struggling to manage your diabetes? The 30-Day Diabetes Reset Program at Dr. Jason Shumard‘s Integrative Wellness Center, founded in 2005, is here to empower you to take charge of your health through safe alternative treatment options. This comprehensive initiative integrates nutritional education, physical activity, and behavior modification strategies, enabling you to manage your condition effectively.
It’s important to recognize that a holistic approach can make a significant difference in understanding diabetes symptoms type 2. This program not only alleviates diabetes symptoms type 2 but also addresses the underlying causes, promoting sustainable health transformations. With personalized coaching and a wealth of resources, you’ll be equipped with the necessary tools for lasting lifestyle changes.
Dr. Jason Shumard, with nearly 20 years of expertise in functional endocrinology and clinical nutrition, emphasizes that lifestyle changes are essential for effectively managing diabetes symptoms type 2 and enhancing overall health results. Many patients find that these changes lead to remarkable improvements. Transformative patient testimonials highlight significant enhancements in metabolic markers and quality of life, showcasing the real-world impact of the program.
One participant shared, “I lost 55 lbs, and my A1C decreased from 9.1 to 5.7 after joining this program.” This demonstrates the program’s potential to reverse type 2 diabetes and promote holistic health. If you’re ready to take the first step toward a healthier you, consider joining us on this journey.
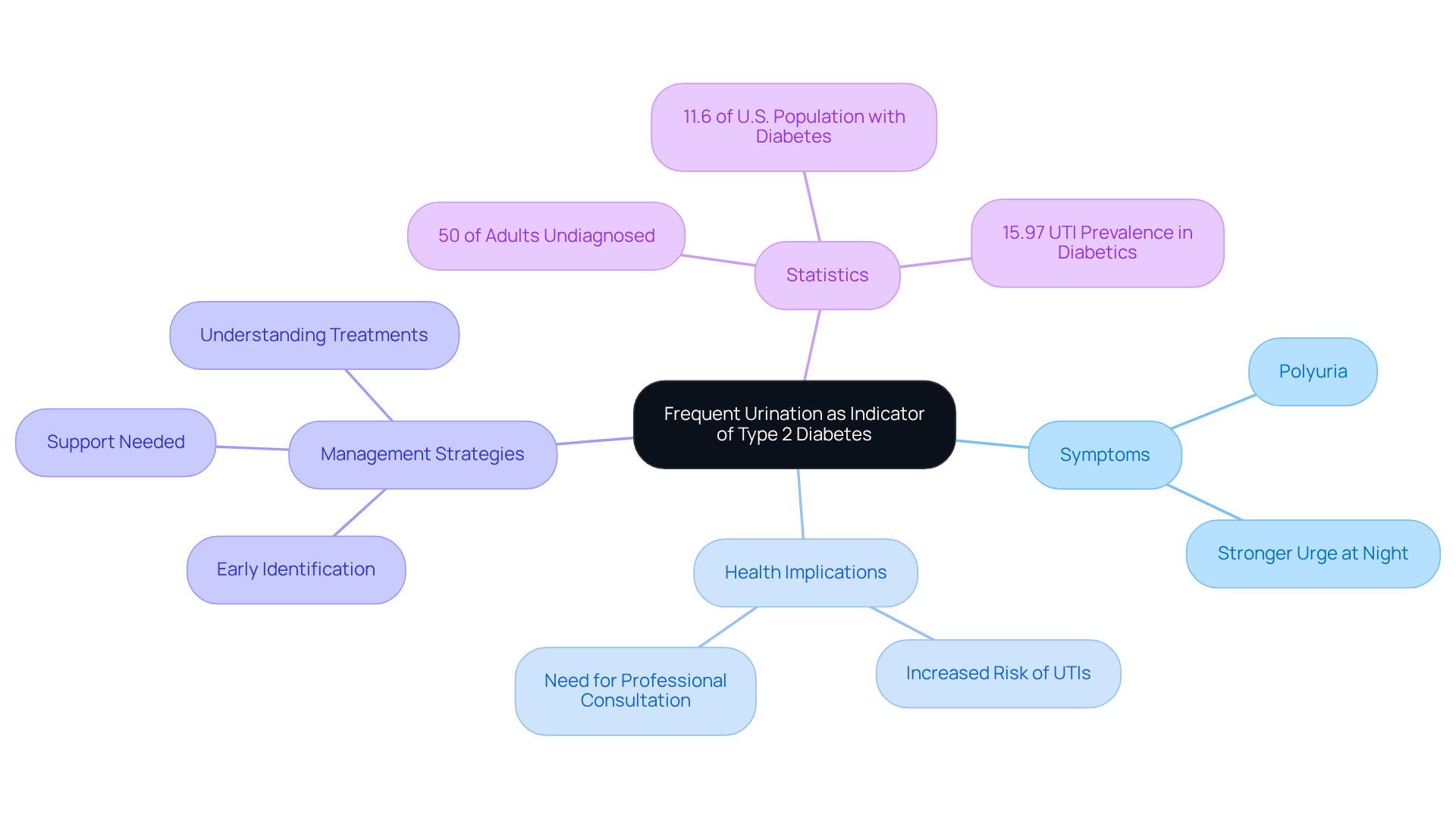
Frequent Urination: A Key Indicator of Type 2 Diabetes
Regular urination, referred to as polyuria, can be a concerning sign of diabetes symptoms type 2. This occurs when your kidneys filter out excess glucose from your blood, leading to increased urine output. Many people experience a stronger urge to urinate, especially at night. It’s crucial to recognize polyuria early on; it can encourage you to consult with a healthcare professional, allowing for timely intervention and better management of blood sugar levels.
Did you know that nearly 50% of adults with elevated blood sugar levels remain undiagnosed? This often happens because diabetes symptoms type 2, like frequent urination, develop gradually. As of 2021, about 11.6% of the U.S. population was living with diabetes symptoms type 2, highlighting the need to identify signs like frequent urination. Addressing this issue promptly can significantly impact your blood sugar control. When glucose levels rise, it leads to increased urine production, as excess glucose in the urine draws in more water.
Frequent urination is not just a symptom; it can also raise the risk of urinary tract infections (UTIs) for those with high blood sugar. It’s important to be aware that some traditional treatments, such as insulin injections, might inadvertently worsen insulin resistance, making management more challenging. By understanding the implications of polyuria and the potential drawbacks of standard therapies, you can take proactive steps toward better health outcomes. Early identification and intervention in managing type 2 diabetes are vital, and you deserve support on this journey.
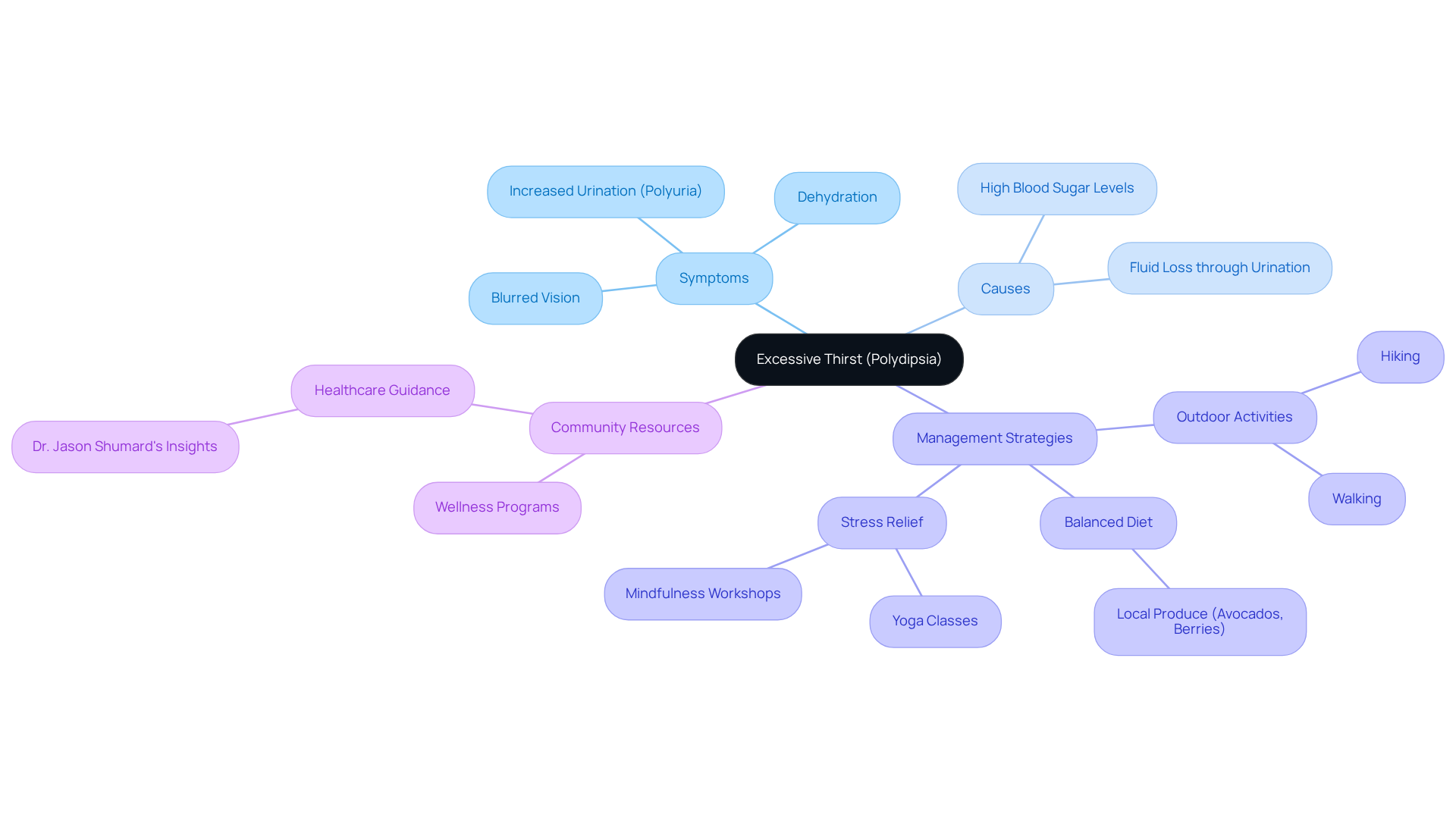
Excessive Thirst: Recognizing a Warning Sign of Type 2 Diabetes
Excessive thirst, known as polydipsia, can be a distressing symptom of diabetes symptoms type 2. When blood sugar levels rise, the body tends to lose more fluid through urination, which can lead to dehydration and an increased sense of thirst. Have you ever found yourself drinking more than usual yet still feeling parched? This can be a critical warning sign of diabetes symptoms type 2, indicating the need for medical evaluation and possible adjustments in diabetes management.
In San Marcos, CA, managing this symptom effectively can be approached holistically. Many individuals find that engaging in regular outdoor activities, such as walking or hiking in the beautiful parks around the area, helps regulate blood sugar levels and improves overall hydration. Additionally, focusing on a balanced diet rich in local produce, like avocados and berries, can significantly support better health outcomes.
Community wellness programs, such as those offered at local health centers, along with personalized guidance from healthcare professionals like Dr. Jason Shumard, can provide essential resources tailored to your individual needs. For stress relief, consider joining local yoga classes or mindfulness workshops available in the community. By incorporating these strategies into your routine, you can enhance your diabetes management and more effectively address diabetes symptoms type 2, including excessive thirst. Remember, you are not alone on this journey; support is available every step of the way.
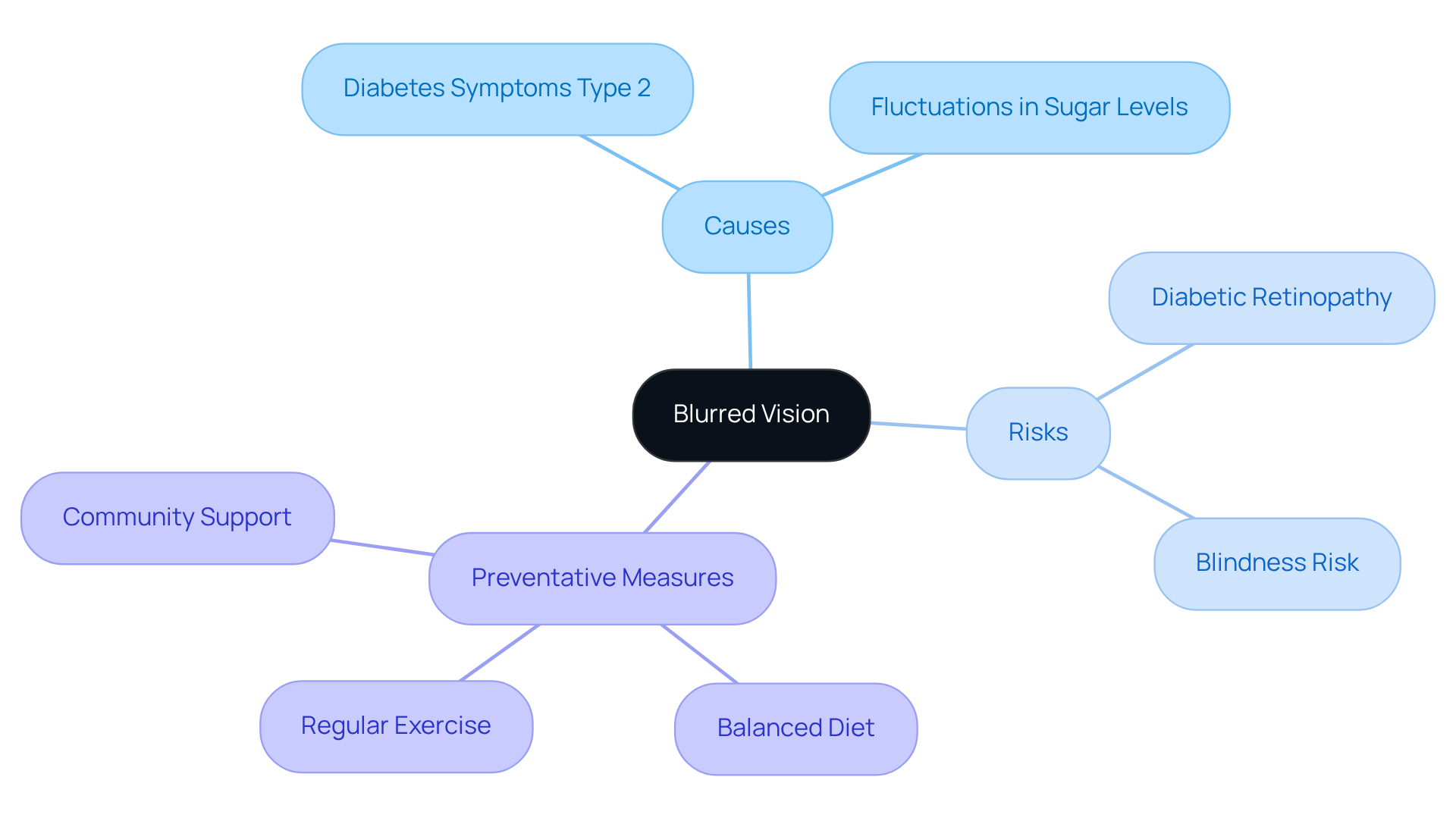
Blurred Vision: A Symptom You Shouldn’t Overlook
Blurred vision is a concerning symptom often associated with diabetes symptoms type 2, which many people experience due to fluctuations in sugar levels. When glucose levels rise, the lens of the eye may swell, causing temporary changes in vision. If these elevated sugar levels persist, they can lead to serious eye conditions, such as diabetic retinopathy, which is a leading cause of blindness among working-age adults. It’s important to recognize that recent studies indicate nearly 30% of individuals with type 2 diabetes may develop diabetic retinopathy after living with the condition for 15 years. Therefore, if you’re experiencing blurred vision, please consult your healthcare provider promptly.
This assessment should focus on both blood sugar control and overall eye health. Effective management can significantly reduce the risk of vision loss. Many patients find that maintaining good metabolic control is crucial for preventing complications related to diabetes symptoms type 2, including those affecting the eyes. Regular eye exams are crucial, as symptoms like blurred vision may not appear until significant damage has occurred.
Incorporating holistic lifestyle strategies can enhance your overall health management. Consider:
- A balanced diet rich in local produce
- Regular outdoor exercise
- The support of your community
These steps can potentially mitigate the risk of complications like blurred vision. Remember, you are not alone in this journey, and taking proactive steps can lead to a healthier future.
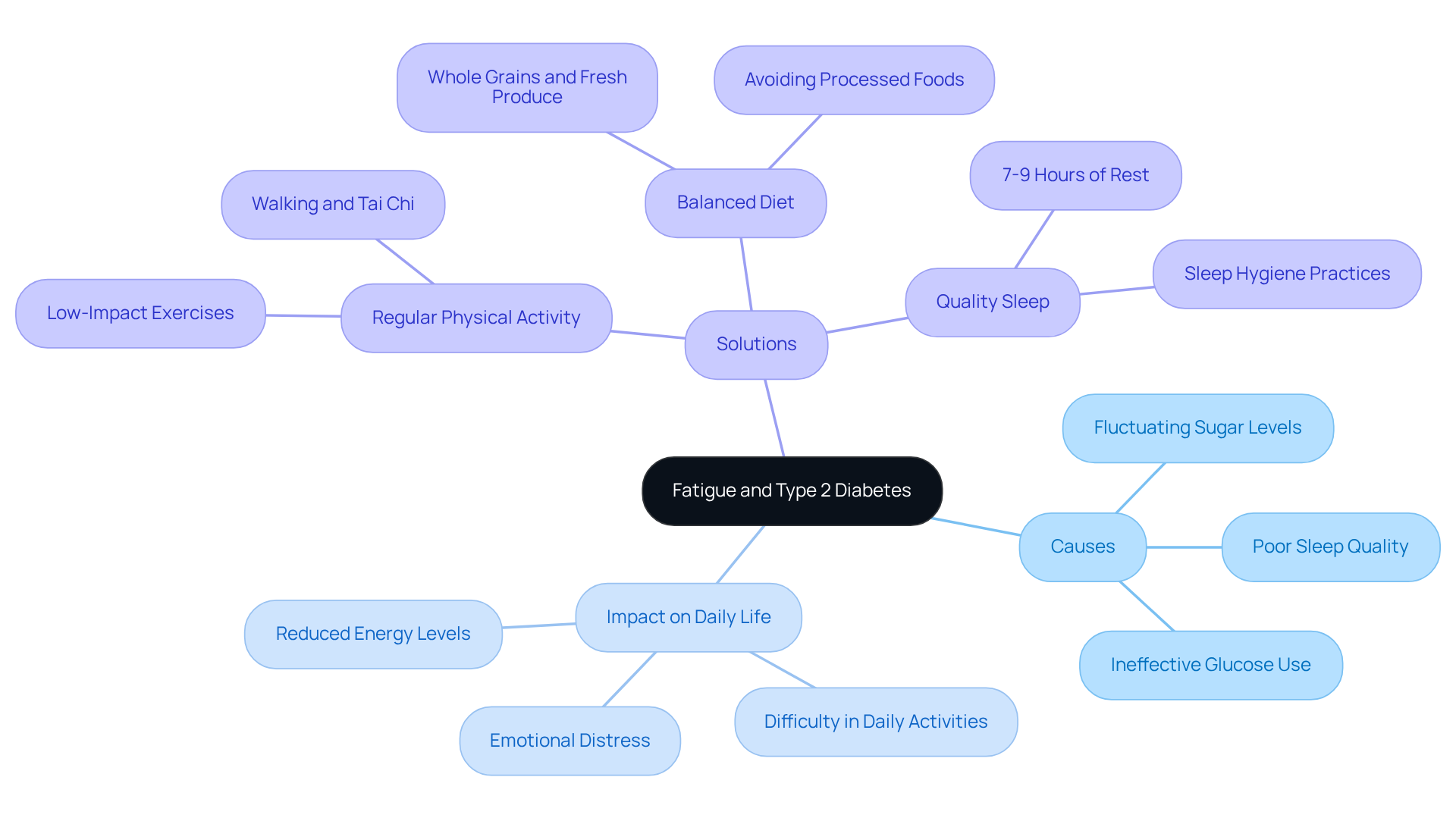
Fatigue: Understanding Its Connection to Type 2 Diabetes
Tiredness is a common challenge for many individuals experiencing diabetes symptoms type 2, often tied to fluctuating sugar levels, poor sleep quality, and the body’s difficulty in using glucose effectively for energy. It’s important to recognize that approximately 61% of patients with diabetes symptoms type 2 report experiencing fatigue, which can greatly impact daily life and overall well-being. Addressing this fatigue requires a comprehensive approach that not only stabilizes sugar levels but also embraces healthy lifestyle changes.
Many patients find that incorporating regular physical activity, such as low-impact exercises, can boost energy levels and enhance glucose metabolism. Additionally, maintaining a balanced diet rich in whole grains and fresh produce is essential for regulating glucose levels and alleviating fatigue symptoms. Real-life stories show that those who make these lifestyle adjustments often report significant improvements in their energy and a decrease in feelings of exhaustion.
Furthermore, healthcare professionals stress the importance of quality sleep, recommending 7-9 hours of rest each night to effectively combat fatigue. By addressing these interconnected factors, individuals experiencing diabetes symptoms type 2 can reclaim their vitality and improve their overall well-being. Remember, every small change can lead to a brighter, more energetic future.
Slow Healing Wounds: A Serious Concern for Diabetes Patients
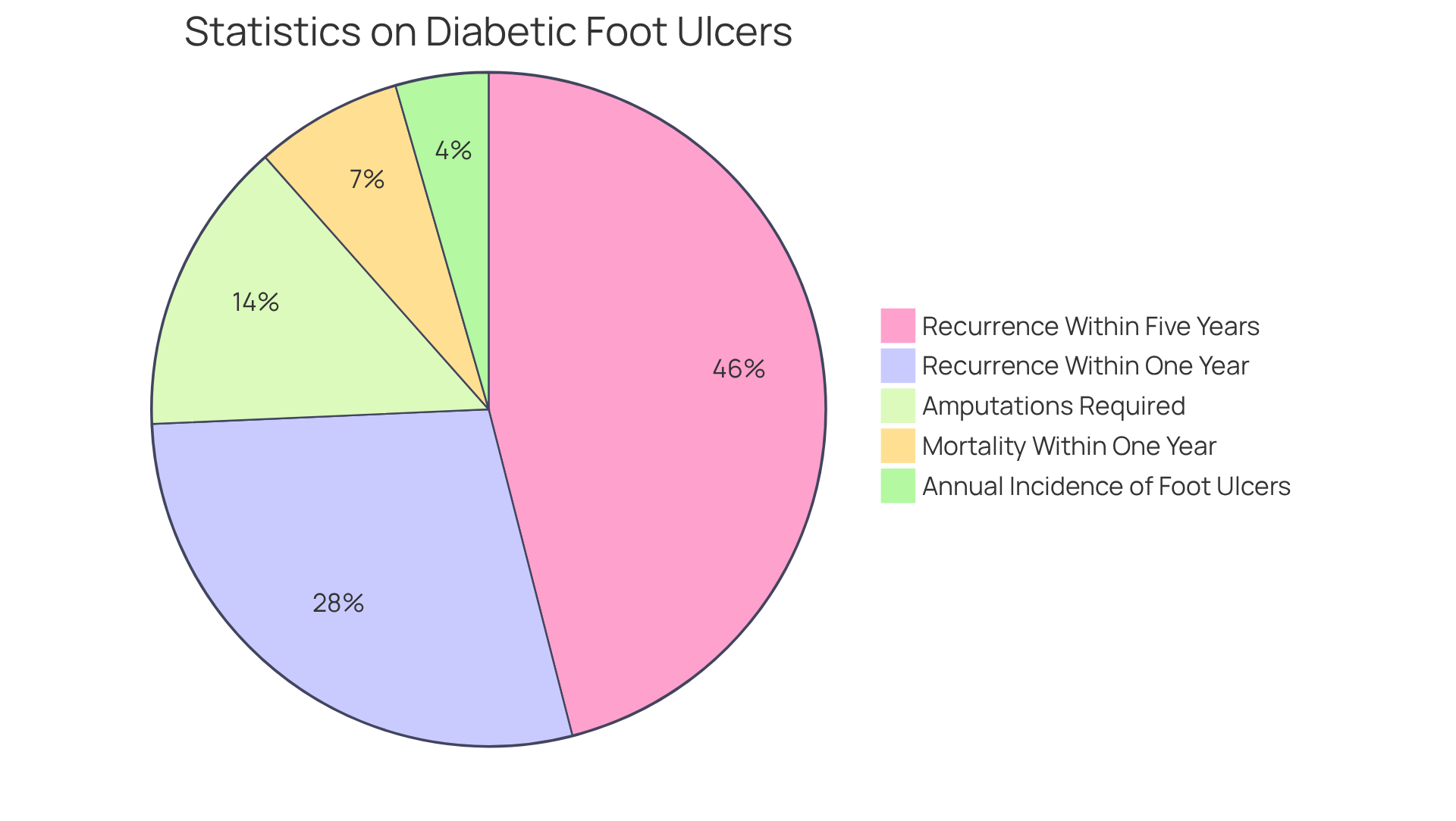
Living with diabetes symptoms type 2 can be incredibly challenging, especially when it comes to managing slow-healing wounds. These wounds often arise from compromised circulation and nerve injury linked to high blood sugar levels. It’s important to recognize that this condition significantly increases the risk of infections and other complications. Studies indicate that nearly 20% of individuals with diabetic foot ulcers may require lower-extremity amputations. Alarmingly, the annual incidence of diabetic foot ulcers is around 6.3% globally, and the mortality rate within one year of the first diagnosis is approximately 10%.
Many patients find that the chronic nature of this issue is underscored by the fact that 65% experience a recurrence of diabetic foot ulcers within five years. This highlights the need for diabetes patients to vigilantly monitor any diabetes symptoms type 2, including wounds, and seek medical attention if healing is delayed. Effective wound care practices are essential to prevent severe complications, as evidenced by the concerning statistic that 40% of patients experience the recurrence of diabetic foot ulcers within just one year of healing. By addressing these issues proactively, you can mitigate risks and enhance your overall health outcomes.
Adopting lifestyle changes can greatly enhance healing and overall well-being. Consider incorporating a balanced diet rich in local produce, engaging in regular outdoor exercise, and practicing stress control. Furthermore, participating in community wellness initiatives in San Marcos can provide invaluable assistance and resources tailored for blood sugar control. As Dr. Jason Shumard emphasizes, “Proper wound care and management are crucial to prevent serious complications.”
For personalized guidance that meets your unique needs, why not reach out to our expert team at Integrative Wellness Center? We’re here to support you on your journey to better health.
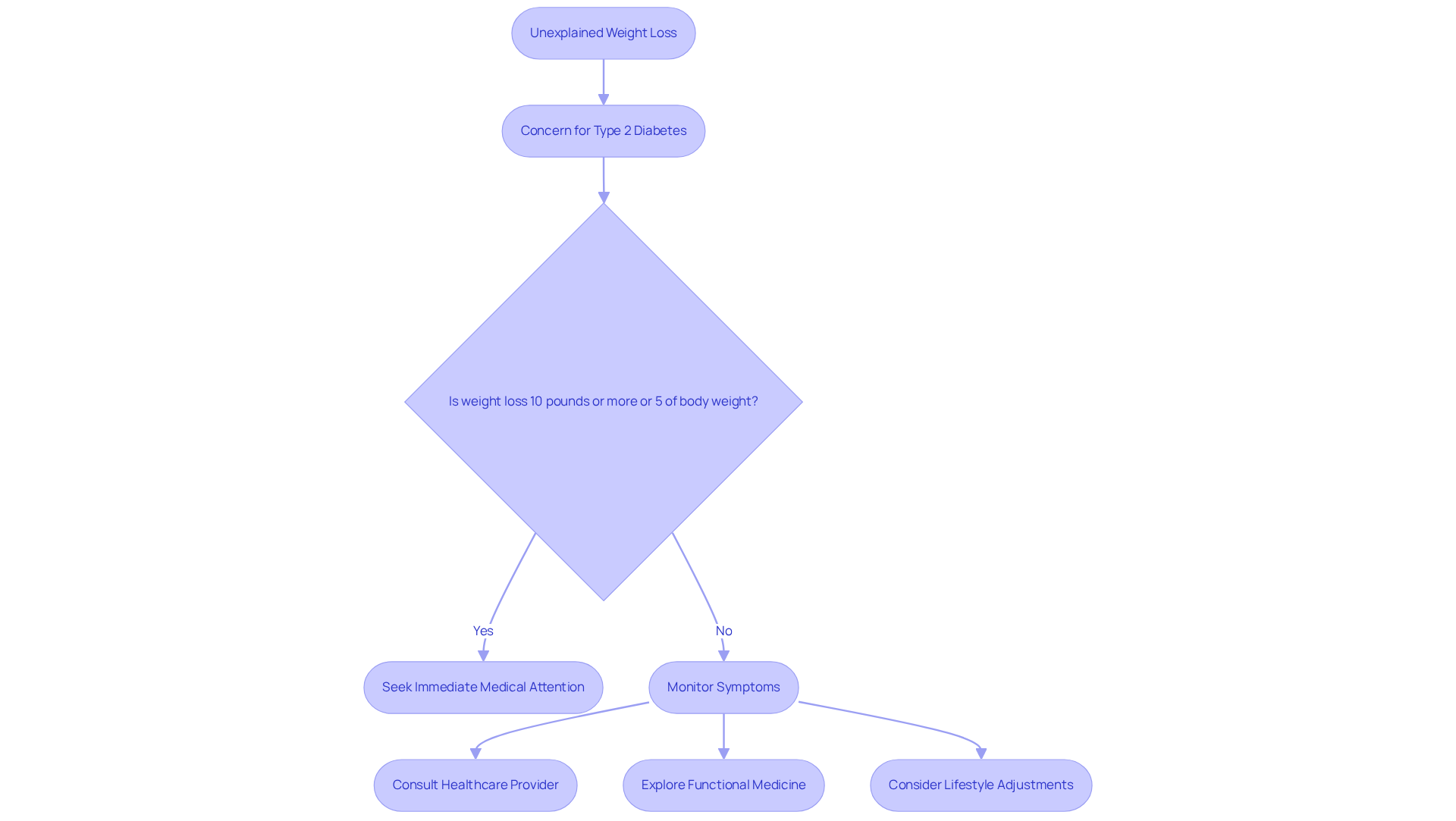
Unexplained Weight Loss: A Symptom of Type 2 Diabetes
Unexplained weight loss can be a significant concern, especially for those dealing with type 2 conditions. Losing weight without any changes in diet or physical activity can be alarming. This happens when the body struggles to use glucose effectively. When blood sugar levels rise, the body often compensates by breaking down fat and muscle for energy, resulting in noticeable weight loss. It’s crucial to recognize that losing 10 pounds or more—or 5% of your body weight—over six to twelve months can signal diabetes symptoms type 2, indicating unmanaged blood sugar issues that need immediate medical attention.
Many individuals may find it unsettling to learn that unexplained weight loss can indicate underlying health problems, such as diabetes symptoms type 2. Research shows that greater weight loss during the first two years of treatment is linked to a higher chance of remission, emphasizing the importance of addressing this symptom early on. If you’re experiencing unexplained weight loss, please consult with your healthcare provider to explore potential causes and receive the care you deserve.
It’s important to acknowledge that traditional treatments for blood sugar regulation, like insulin injections, might unintentionally worsen insulin resistance, complicating management efforts. Dr. Shumard’s comprehensive approach emphasizes education and empowerment, guiding patients to explore individualized functional medicine strategies. This focus on customized nutrition and lifestyle adjustments can lead to a more effective way to manage blood sugar. Remember, you’re not alone in this journey—support is available, and taking proactive steps can make a significant difference in your health.
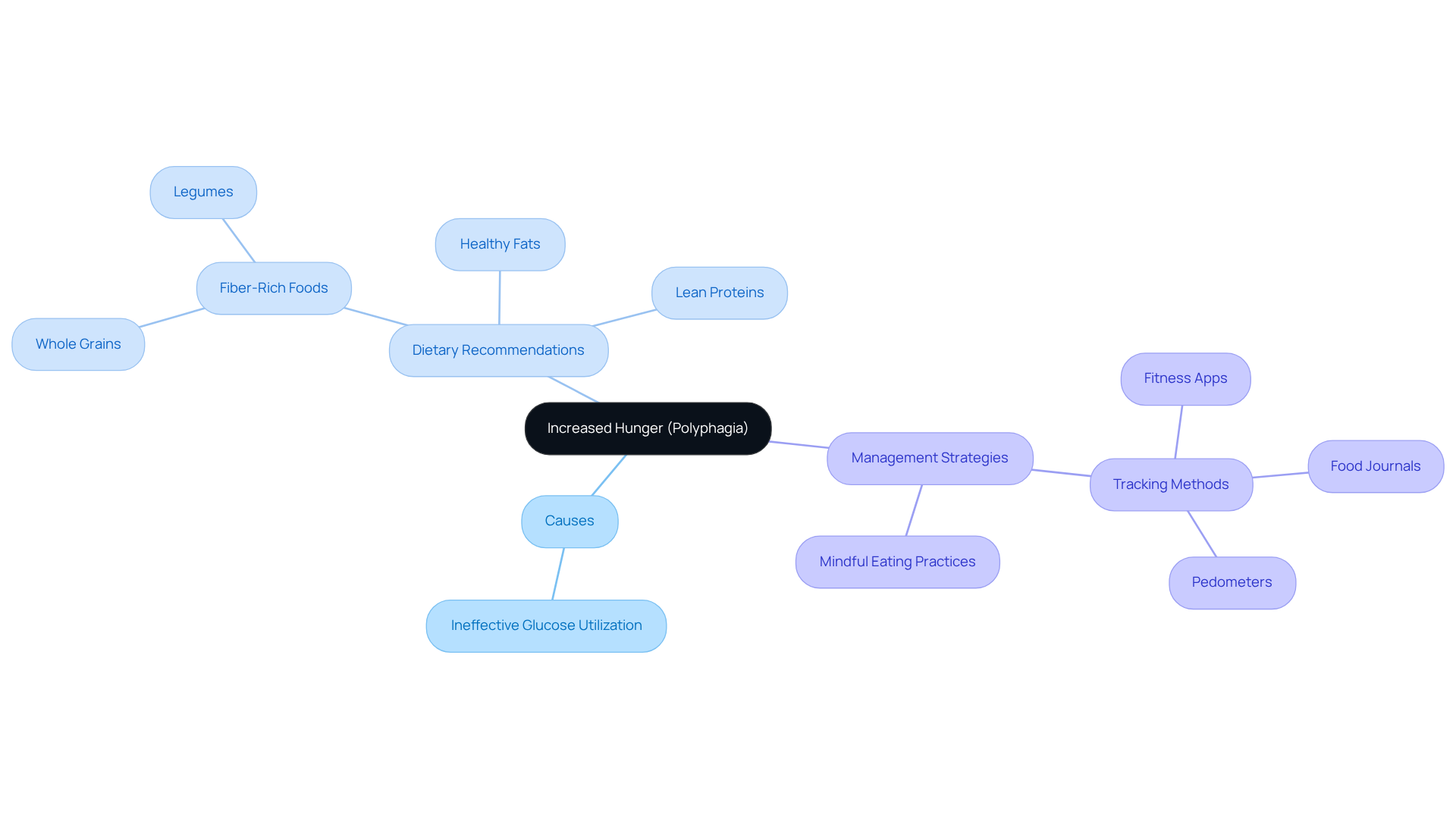
Increased Hunger: A Sign of Potential Diabetes Issues
Heightened appetite, or polyphagia, is a common challenge faced by individuals experiencing diabetes symptoms type 2. This arises from the body’s struggle to utilize glucose effectively for energy, leading to a persistent feeling of hunger. It’s important to recognize that this ongoing sensation can lead to overeating and poor dietary choices, making it even more difficult to manage blood sugar levels. Current data reveals that nearly 90-95% of diabetes cases in the U.S. are type 2, underscoring the prevalence of diabetes symptoms type 2 such as polyphagia within this community.
Managing polyphagia requires a thoughtful approach to your eating habits and goal-setting. Nutritionists often suggest focusing on balanced meals that include:
- Fiber-rich foods
- Lean proteins
- Healthy fats
These elements can enhance your sense of fullness and help stabilize glucose levels. For instance, incorporating whole grains, legumes, and a variety of vegetables can significantly reduce the urge to eat constantly. Many patients find that utilizing tracking methods—such as fitness apps, journals, or pedometers—can greatly enhance accountability and help monitor their progress.
Real-world examples highlight the successful management of polyphagia through mindful eating practices and structured goal-setting. One patient shared that by planning meals weekly and maintaining a food journal, they were able to lower their hunger levels and achieve better blood sugar control. Furthermore, educational resources, such as those offered by Dr. Jason Shumard’s center, empower patients with essential knowledge about their conditions, enabling informed dietary choices and realistic health goals.
Nutritionists emphasize the importance of tuning into your body’s signals. As one specialist notes, ‘Identifying the distinction between genuine hunger and cravings is essential for effective management of the condition.’ By addressing polyphagia through informed dietary adjustments and structured goal-setting, you can take meaningful steps toward improved health outcomes and a better quality of life.
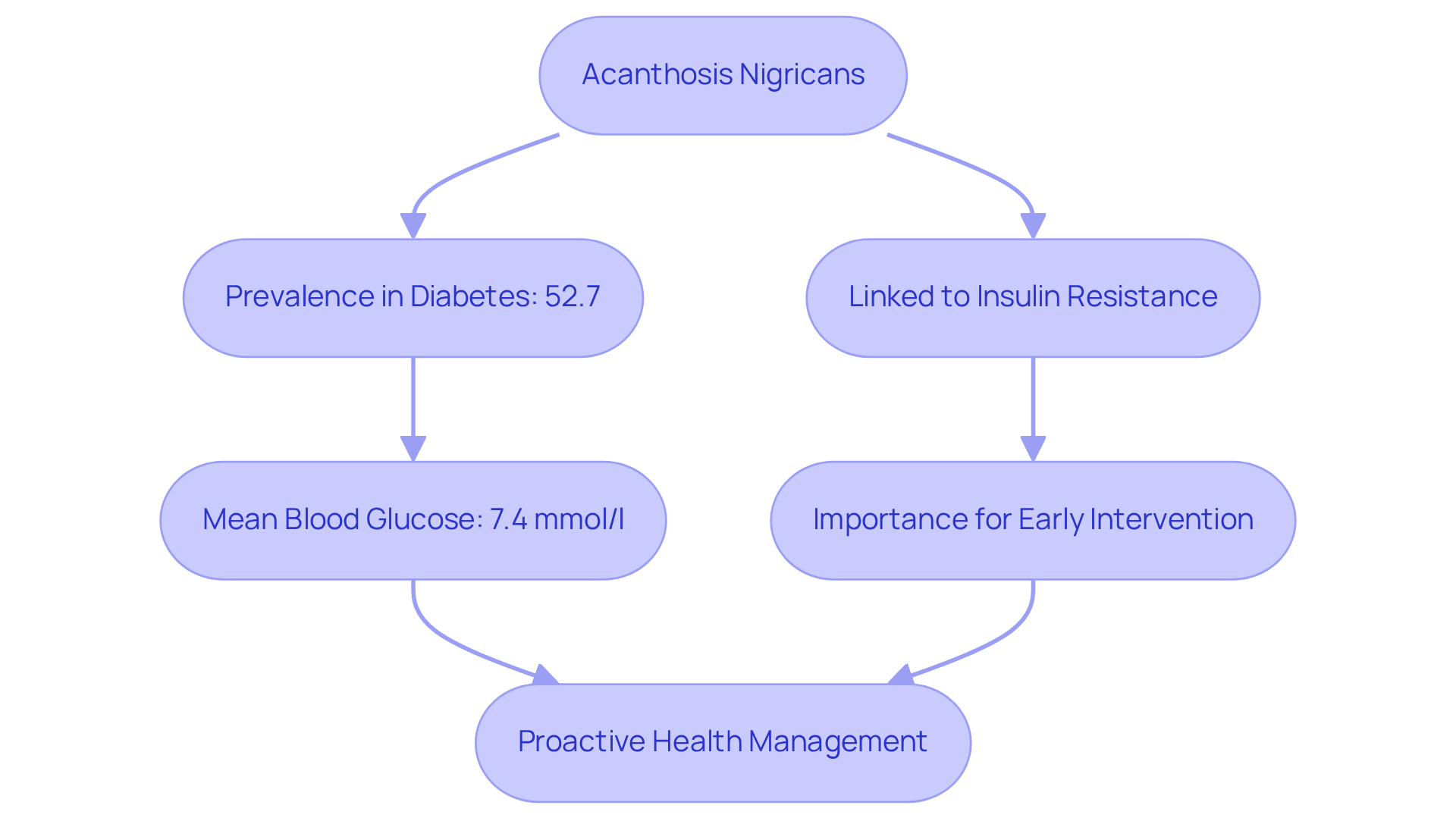
Dark Patches of Skin: A Visual Symptom of Type 2 Diabetes
Acanthosis nigricans, often marked by dark patches of skin, typically appears in areas such as the neck, armpits, and groin. This skin condition is closely linked to insulin resistance and may serve as an early sign of diabetes symptoms type 2. Research indicates that up to 52.7% of diabetic individuals may experience acanthosis nigricans, highlighting its importance in evaluating health risks. It’s crucial to recognize these skin changes, as they can encourage individuals to seek medical evaluation and address underlying metabolic issues. For instance, studies show that individuals with acanthosis nigricans have a mean random blood glucose level of 7.4 mmol/l, compared to 6.7 mmol/l in those without the condition. This underscores the significance of acanthosis nigricans not just as a visible indicator, but also as a prompt for early intervention.
The American Diabetes Association acknowledges acanthosis nigricans as a risk factor for diabetes symptoms type 2, further emphasizing the need for awareness. By recognizing and pinpointing diabetes symptoms type 2, patients can take proactive steps towards managing their health and potentially reversing the progression of type 2 diabetes. It’s important to understand that traditional therapies may unintentionally worsen insulin resistance. Therefore, a comprehensive strategy for managing the condition, like that advocated by Dr. Jason Shumard, becomes essential for effective care.
Moreover, many patients have shared their experiences, emphasizing the dangers associated with traditional therapies. This reinforces the necessity for a more tailored and comprehensive approach to managing the condition, especially considering safety concerns in healthcare settings. By fostering a deeper understanding of acanthosis nigricans, we can empower individuals to take charge of their health and embark on a journey toward well-being.
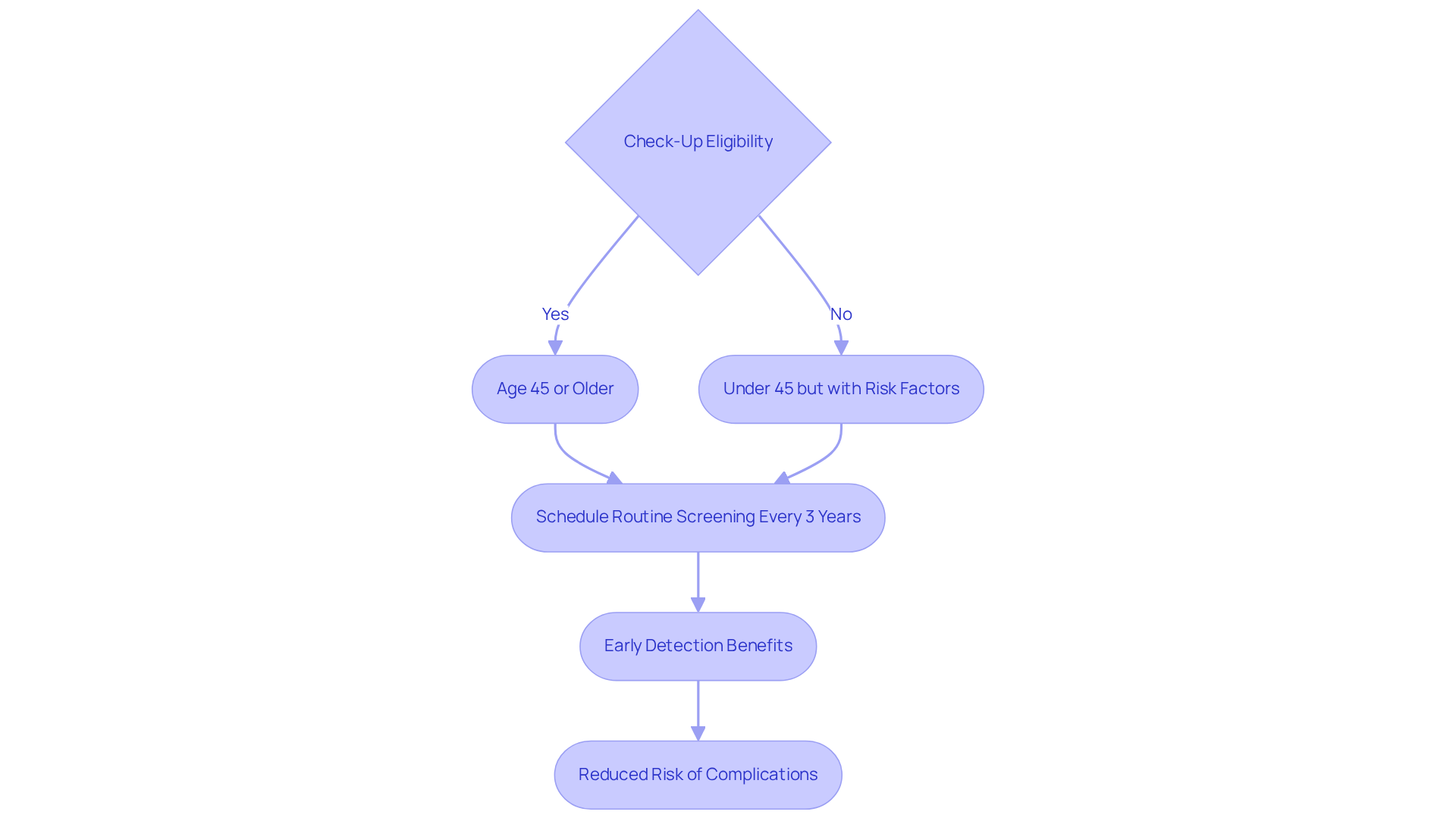
Regular Check-Ups: Essential for Early Detection of Diabetes Symptoms
Routine check-ups are not just necessary; they are vital for individuals experiencing diabetes symptoms type 2 or those at risk. These visits help track blood sugar levels and overall health, allowing healthcare providers to catch any developing complications early. This early recognition is crucial for effective management.
It’s important to recognize that current guidelines suggest adults aged 45 and older, or those with risk factors like obesity or a family history of diabetes symptoms type 2, should have routine screenings at least every three years. Many patients find that early detection through these screenings can significantly improve their health outcomes. For instance, individuals diagnosed early are more likely to manage their condition effectively and steer clear of severe complications such as heart disease or kidney failure.
In fact, studies show that timely interventions can reduce the risk of diabetes-related complications by up to 50%. Therefore, maintaining regular appointments is essential for proactive health management. By addressing any potential issues promptly, you take a significant step toward a healthier future. Remember, you’re not alone on this journey; support is always available.
Conclusion
Recognizing and addressing the symptoms of type 2 diabetes is crucial for effective management and improved health outcomes. It’s important to understand that early detection can make a significant difference. This article highlights ten significant symptoms that should not be overlooked, emphasizing the importance of taking proactive steps toward better health. By recognizing these signs, individuals can potentially reverse the progression of diabetes and improve their overall well-being.
Many patients find that frequent urination and increased thirst are key indicators of elevated blood sugar levels. Other symptoms, such as:
- Blurred vision
- Fatigue
- Slow-healing wounds
- Unexplained weight loss
further illustrate the multifaceted nature of diabetes. Regular check-ups and a holistic approach to management—including lifestyle changes and community support—are essential for enhancing one’s quality of life.
Ultimately, awareness and education are vital in the journey toward managing diabetes. By recognizing these symptoms and seeking appropriate support, you can take charge of your health. Have you considered engaging in wellness programs, such as the 30-Day Diabetes Reset Program? Empowering yourself with knowledge and resources can lead to lasting health transformation. Taking these steps not only improves your personal health but also contributes to a broader understanding of diabetes management within the community.
Frequently Asked Questions
What is the 30-Day Diabetes Reset Program at the Integrative Wellness Center?
The 30-Day Diabetes Reset Program is a comprehensive initiative designed to help individuals manage their diabetes through nutritional education, physical activity, and behavior modification strategies, promoting sustainable health transformations.
Who founded the Integrative Wellness Center and what is their expertise?
The Integrative Wellness Center was founded by Dr. Jason Shumard, who has nearly 20 years of expertise in functional endocrinology and clinical nutrition.
How does the program approach diabetes management?
The program takes a holistic approach by addressing both the symptoms and underlying causes of type 2 diabetes, providing personalized coaching and resources for lasting lifestyle changes.
What kind of results have participants experienced from the program?
Participants have reported significant improvements in their health, including weight loss and better metabolic markers. For example, one participant lost 55 lbs and decreased their A1C from 9.1 to 5.7.
What is polyuria and how is it related to type 2 diabetes?
Polyuria is a condition characterized by frequent urination, which occurs when kidneys filter excess glucose from the blood. It is a common symptom of type 2 diabetes and can indicate the need for medical evaluation.
Why is it important to recognize polyuria early?
Early recognition of polyuria can lead to timely intervention and better management of blood sugar levels, which is crucial since nearly 50% of adults with elevated blood sugar remain undiagnosed.
What complications can arise from frequent urination in individuals with high blood sugar?
Frequent urination can increase the risk of urinary tract infections (UTIs) for those with high blood sugar levels.
What is polydipsia and how does it relate to diabetes?
Polydipsia is excessive thirst that occurs when blood sugar levels rise, leading to fluid loss through urination and dehydration. It is a warning sign of type 2 diabetes that requires medical evaluation.
How can individuals manage excessive thirst related to diabetes?
Effective management can include engaging in regular outdoor activities, maintaining a balanced diet rich in local produce, and participating in community wellness programs. Personalized guidance from healthcare professionals can also be beneficial.
What support is available for individuals managing diabetes symptoms?
Individuals can access community wellness programs, personalized guidance from healthcare professionals, and local activities like yoga classes or mindfulness workshops to enhance their diabetes management.